|
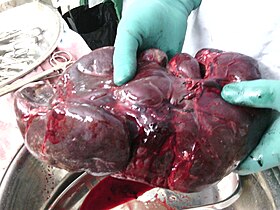
Splenectomy
A splenectomy is the surgical procedure that partially or completely removes the spleen. The spleen is an important organ in regard to immunological function due to its ability to efficiently destroy encapsulated bacteria. Therefore, removal of the spleen runs the risk of overwhelming post-splenectomy infection, a medical emergency and rapidly fatal disease caused by the inability of the body's immune system to properly fight infection following splenectomy or asplenia.[1] Common indications for splenectomy include trauma, tumors, splenomegaly or for hematological disease such as sickle cell anemia or thalassemia.[2] IndicationsThe spleen is an organ located in the abdomen next to the stomach. It is composed of red pulp which filters the blood, removing foreign material, damaged and worn out red blood cells. It also functions as a storage site for iron, red blood cells and platelets. The rest (~25%) of the spleen is known as the white pulp and functions like a large lymph node being the largest secondary lymphoid organ in the body.[3] Apart from regular lymphatic function the white pulp contains splenic macrophages which are particularly good at destroying (phagocytosis) encapsulated bacteria such as Streptococcus pneumoniae.[4] The spleen is also known to function as a site for the development of new red blood cells from their hematopoietic stem cell precursors, and particularly in situations in which the bone marrow, the normal site for this process, has been compromised by a disorder such as leukemia. The spleen is enlarged in a variety of conditions such as malaria, mononucleosis and most commonly in cancers of the lymphatics, such as lymphomas or leukemia. It is removed under the following circumstances:
The classical cause of traumatic damage to the spleen is a blow to the abdomen during a sporting event. In cases where the spleen is enlarged due to illness (mononucleosis), trivial activities, such as leaning over a counter or straining while defecating, can cause a rupture. ProcedureLaparoscopy is the preferred procedure in cases where the spleen is not too large and when the procedure is elective. Open surgery is performed in trauma cases or if the spleen is enlarged. Either method is major surgery and is performed under general anesthesia. Vaccination for S. pneumoniae, H. influenza and N. meningitidis should be given pre-operatively if possible to minimize the chance of overwhelming post-splenectomy infection (OPSI), a rapid-developing and highly fatal type of septicaemia. The spleen is located and disconnected from its arteries. The ligaments holding the spleen in place, gastrosplenic ligament, splenorenal ligament and splenocolic ligament, are dissected and the organ is removed. In some cases, one or more accessory spleens are discovered and also removed during surgery. The incisions are closed and when indicated, a drain is left. If necessary, tissue samples are sent to a laboratory for analysis.[citation needed] Side effectsSplenectomy causes an increased risk of sepsis, particularly overwhelming post-splenectomy sepsis due to encapsulated organisms such as S. pneumoniae and Haemophilus influenzae which are no longer able to be destroyed.[4] It has been found that the risk of acquiring sepsis is 10 to 20 times higher in a splenectomized patient compared to a non-splenectomized patient, which can result in death, especially in young children.[6] Therefore, patients are administered the pneumococcal conjugate vaccine (Prevnar), Hib vaccine, and the meningococcal vaccine post-operatively (see asplenia). These bacteria often cause a sore throat under normal circumstances but after splenectomy, when infecting bacteria cannot be adequately opsonized, the infection becomes more severe.[citation needed] Splenectomy also increases the severity of babesiosis, Splenectomized patients are more susceptible to contracting babesiosis and can die within five to eight days of symptom onset.[7] They have severe hemolytic anemia, and occasional hepatomegaly has been documented. Parasitemia levels can reach up to 85% in patients without spleens, compared to 1–10% in individuals with spleens and effective immune systems.[8] An increase in blood leukocytes can occur following a splenectomy.[9] The post-splenectomy platelet count may rise to abnormally high levels (thrombocytosis), leading to an increased risk of potentially fatal clot formation. Mild thrombocytosis may be observed after a splenectomy due to the lack of sequestering and destruction of platelets that would normally be carried out by the spleen. In addition, the splenectomy may result in a slight increase in the production of platelets within the bone marrow. Normally, erythrocytes are stored and removed from the circulating blood by the spleen, including the removal of damaged erythrocytes. However, after a splenectomy the lack of presence of the spleen means this function cannot be carried out so damaged erythrocytes will continue to circulate in the blood and can release substances into the blood. If these damaged erythrocytes have a procoagulant activity then the substances they release can lead to the development of a procoagulant state and this can cause thromboembolic events e.g. pulmonary embolism, portal vein thrombosis and deep vein thrombosis.[6] There also is some conjecture that post-splenectomy patients may be at elevated risk of subsequently developing diabetes.[10] Splenectomy may also lead to chronic neutrophilia. Splenectomy patients typically have Howell-Jolly bodies[11][12] and less commonly Heinz bodies in their blood smears.[13] Heinz bodies are usually found in cases of G6PD (Glucose-6-Phosphate Dehydrogenase) and chronic liver disease.[14] A splenectomy also results in a greatly diminished frequency of memory B cells.[15] A 28-year follow-up of 740 World War II veterans who had their spleens removed on the battlefield showed a significant increase in the usual death from pneumonia (6 deaths rather than the expected 1.74) and an increase in the deaths from ischemic heart disease (41 deaths rather than the expected 30.26) but not from other conditions.[16] Subtotal splenectomyMuch of the spleen's protective roles can be maintained if a small amount of spleen can be left behind.[17] Where clinically appropriate, attempts are now often made to perform either surgical subtotal (partial) splenectomy,[18] or partial splenic embolization.[19] In particular, whilst vaccination and antibiotics provide good protection against the risks of asplenia, this is not always available in poorer countries.[20] However, as it may take some time for the preserved splenic tissue to provide the full protection, it has been advised that preoperative vaccination still be given.[21] See also
References
|
||||||||||||